
“
Chronic pain and mental health are deeply intertwined. When pain persists beyond normal healing time, it can lead to emotional distress, reduced quality of life, and even psychological disorders. Many individuals suffering from chronic pain often experience anxiety, depression, and social isolation, making it more than just a physical issue. 1
1
”
Studies show that individuals with chronic pain are three times more likely to develop depression than those without, highlighting a strong psychological burden that extends far beyond physical discomfort. 1
Anxiety often increases with chronic pain because the brain is in a constant state of alert. This ongoing stress response can heighten pain perception, creating a cycle of tension and discomfort. 2

Chronic pain frequently disrupts sleep quality. This leads to insomnia or non-restorative sleep, which negatively impacts cognitive function, emotional stability, and resilience against everyday mental stressors.
People with long-term pain often experience emotional burnout. The continuous effort to cope can lead to feelings of hopelessness, withdrawal, and low self-worth, deeply affecting mental well-being. 3
Persistent pain can change how the brain processes emotions and pain signals. Over time, pain can become magnified because the nervous system becomes more sensitive to even minor discomforts. 4
Chronic pain sufferers may avoid social interaction due to fatigue, mobility issues, or embarrassment, leading to isolation. Loneliness then worsens depression and creates a sense of emotional disconnection. 5
Fear of worsening pain or injury often limits activity, reinforcing avoidance behaviors. This cycle can diminish confidence, increase anxiety, and promote a more negative view of life and self-worth. 6
A lack of proper diagnosis or understanding from others may cause chronic pain sufferers to feel invalidated. This can result in emotional distress and damaging both relationships and mental stability. 7
Brain imaging shows chronic pain affects neurotransmitters like serotonin and dopamine, which are vital to mood regulation. These changes may result in mood swings, sadness, or emotional numbness. 8

Chronic pain patients often report cognitive fog—difficulty concentrating or remembering. This “pain fog” impairs daily function and contributes to frustration, confusion, and a growing sense of helplessness.
Financial stress from medical expenses, reduced income, or job loss due to pain intensifies anxiety and depression. Economic pressure silently worsens emotional health in chronic pain patients. 9
The constant need to explain or justify one’s invisible pain can lead to mental fatigue. This defensive mindset can increase irritability, anxiety, and feelings of being misunderstood or alone. 10
The frustration of failed treatments or slow recovery often leads to emotional exhaustion. Over time, this disillusionment may result in hopelessness or a belief that life will never return to normal. 11
Philosopher Friedrich Nietzsche once wrote, “To live is to suffer; to survive is to find meaning in the suffering.” This insight reminds us that managing chronic pain requires emotional healing.12
People with chronic pain frequently experience distorted body image or self-perception, feeling they are “broken.” These thoughts often lead to reduced confidence, embarrassment, and depression. 13
Substance misuse can develop as some individuals turn to painkillers or alcohol to manage discomfort and stress. Over time, this behavior can further impair mental health and cause dependency. 14
Chronic pain often affects a person’s identity. When roles shift—from worker to patient, or parent to dependent—it can cause grief, frustration, and loss of self-worth, damaging emotional resilience.
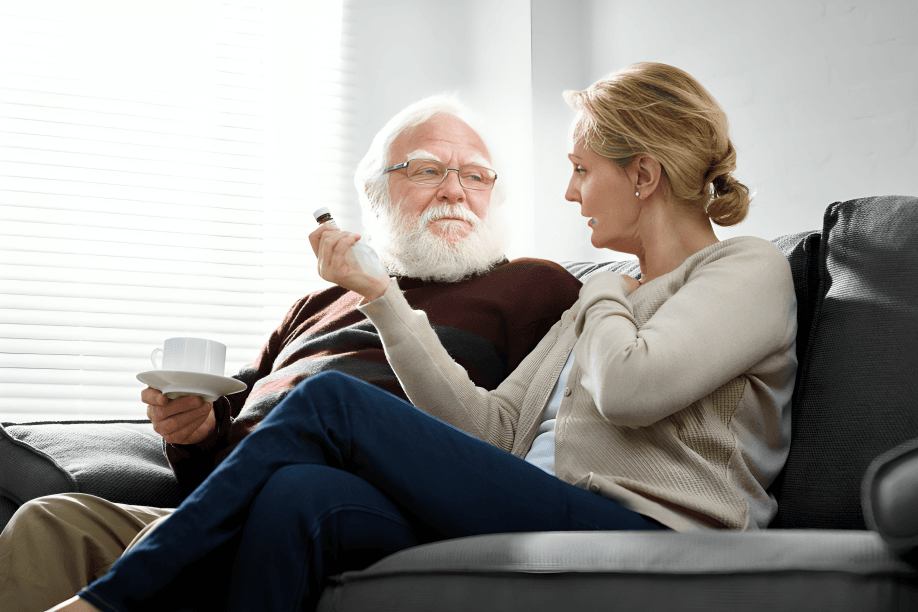
Emotional support is critical. Patients with strong social networks or involved family and friends often report better mood regulation, lower anxiety, and improved coping skills compared to isolated individuals. 15
The unpredictability of pain flares can cause constant worry. This uncertainty feeds stress and fear, reducing life satisfaction and making it hard to plan for the future or enjoy the present. 16
Cultural and societal stigma around invisible illnesses can add emotional strain. Feeling judged or disbelieved can intensify mental distress, especially when pain is not visibly evident to others. 17


