
“
Chronic pain management involves a wide range of approaches aimed at reducing long-term pain and improving life quality. From medical therapies to holistic practices, chronic pain management is a vital healthcare focus that requires consistent and personalized strategies. 1
1
”
Ancient Greek physician Hippocrates used willow bark for pain relief, unknowingly tapping into salicin—an ingredient later used in aspirin—marking one of the earliest efforts in chronic pain management. 1
Chronic pain management often starts with identifying the pain’s root cause, as treating the underlying issue—rather than just symptoms—can lead to more effective and sustainable results over time. 2
Cognitive behavioral therapy (CBT) is proven to help chronic pain sufferers by changing thought patterns, managing emotional responses, and teaching coping skills that significantly reduce perceived pain levels. 3
Anti-inflammatory medications, such as NSAIDs, are frequently prescribed for chronic pain, particularly where inflammation is present, offering temporary relief and forming part of a broader pain strategy.
Massage therapy can reduce muscle tension, enhance circulation, and release endorphins—all of which help to alleviate chronic pain, particularly in the back, neck, and shoulders. 4
Regular aerobic exercise—even low-impact activities like walking or swimming—can boost endorphin production and reduce chronic pain severity through enhanced blood flow and overall physical conditioning. 5
Sleep hygiene is a critical but often overlooked aspect of pain management, as chronic pain and poor sleep often create a feedback loop, each worsening the other without intervention. 6
Diet also influences chronic pain, with anti-inflammatory foods such as leafy greens, berries, and fatty fish shown to help reduce systemic inflammation and, consequently, ongoing pain sensations. 7
Electrical stimulation, such as TENS therapy, offers non-invasive relief for localized pain by disrupting pain signals and encouraging the release of natural painkillers like endorphins in the body. 8

Support groups and chronic pain communities provide emotional strength, shared experiences, and tips, all of which contribute to a more positive outlook and better overall management of persistent pain.
Stress management techniques, including yoga and breathing exercises, reduce muscle tension and cortisol levels—factors that are often responsible for amplifying chronic pain in the body and mind. 9
Neuromodulation technologies, like spinal cord stimulators, are increasingly used to interrupt pain signals at the spinal level, especially when other pain management strategies have proven ineffective. 10
Biofeedback allows chronic pain patients to gain control over bodily functions like muscle tension and heart rate, helping them to manage pain responses with real-time feedback and mental training. 11
Guided imagery, a mind-body technique, uses visualization to redirect focus away from pain and toward calm and healing images, creating a psychological shift that can lessen pain intensity. 12
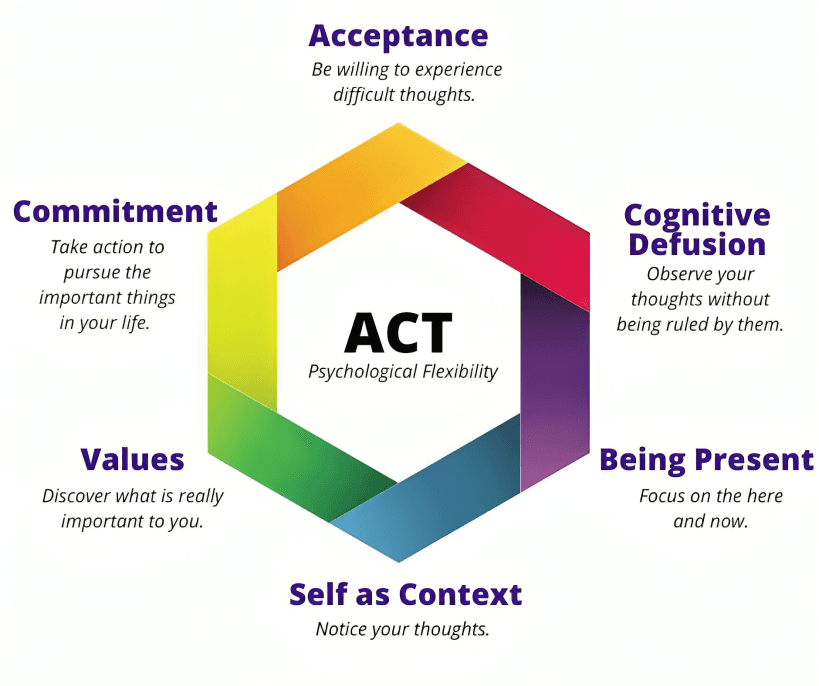
Acceptance and Commitment Therapy (ACT) helps patients to stop resisting pain and instead commit to value-based living despite discomfort, making it an increasingly used strategy in clinical settings.
Heat and cold therapies remain simple yet effective solutions in chronic pain care, helping to reduce inflammation, soothe sore tissues, or numb sharp pain, depending on the specific condition. 13
Occupational therapy helps individuals with chronic pain adjust daily activities to minimize discomfort while maximizing function, often using adaptive tools and techniques for sustainable living. 14
Ketamine infusions, once reserved for anesthesia, are now being explored for chronic pain conditions like CRPS and fibromyalgia due to their ability to reset certain pain pathways in the brain. 15
Vitamin D deficiency has been linked with increased pain levels, especially in musculoskeletal disorders, making supplementation or sun exposure a consideration for managing persistent discomfort. 16
Modern-day pain philosophers and medical ethicists argue for personalized care models, stressing that every chronic pain journey is unique and requires compassion and flexible treatments over rigid protocols. 17


