
“
Living with chronic pain and mental health challenges can feel like an unending battle, as physical discomfort often leads to emotional distress. The link between chronic pain and mental health is deeply intertwined—persistent pain can heighten anxiety, depression, and fatigue, while emotional suffering can worsen pain perception. 1
1
”
Greek physician Hippocrates once noted that pain disturbs the soul. Today, science confirms chronic pain disrupts neurotransmitters, impairing mood regulation and contributing to long-term mental health issues. 1
People with chronic pain are four times more likely to experience depression than those without it, as pain-related sleep loss, isolation, and helplessness contribute to mood disorders over time. 2
Anxiety often increases with chronic pain due to fear of flare-ups, treatment failures, or dependency, creating a cycle where stress amplifies pain signals and impairs overall functioning. 3
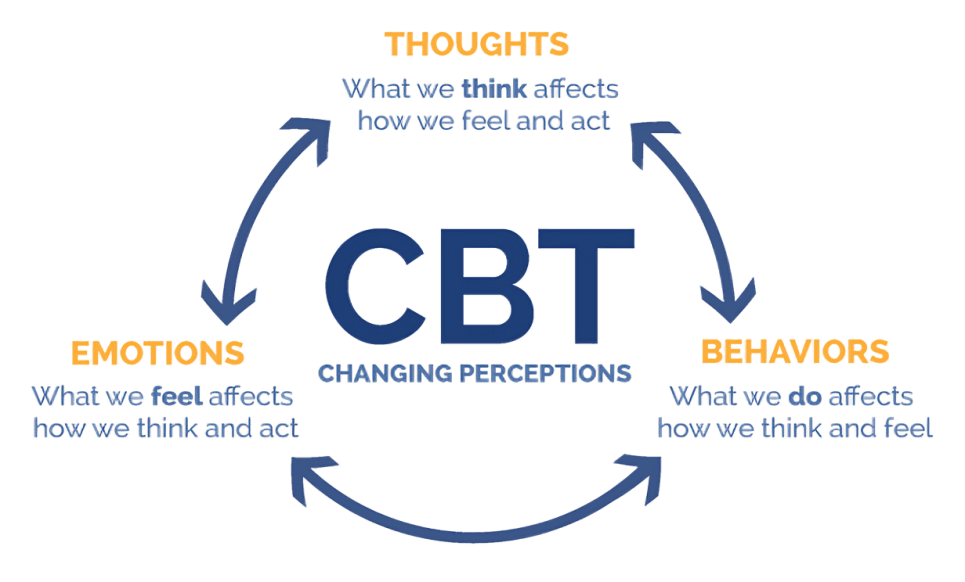
Cognitive Behavioral Therapy (CBT) is widely used to help patients reframe pain-related thoughts, reduce catastrophizing, and promote healthier coping habits despite ongoing physical discomfort.
Social isolation caused by chronic pain can lead to feelings of loneliness and low self-worth, intensifying the mental health toll and making it harder for sufferers to seek emotional support. 4
Brain scans show that chronic pain rewires certain areas related to emotions and memory, particularly the prefrontal cortex and amygdala, leading to long-term psychological effects. 5
Individuals suffering from chronic pain may struggle with identity loss as they can no longer perform former roles or hobbies, which further contributes to feelings of grief and low mood. 6
Relaxation techniques like deep breathing, progressive muscle relaxation, or guided imagery help lower the stress hormone cortisol and can reduce both perceived pain and emotional exhaustion. 7
Chronic pain is associated with a higher risk of suicidal thoughts, particularly when patients feel unheard or untreated, underlining the urgent need for integrated physical and mental healthcare. 8
Sleep disturbances are common in chronic pain sufferers, and poor sleep not only worsens pain sensitivity but also increases emotional instability and mental fatigue during waking hours. 9

Emotional support animals have shown effectiveness in reducing loneliness, decreasing anxiety levels, and even helping distract individuals from persistent pain through companionship and routine.
Mindfulness meditation helps reduce pain intensity by training the brain to observe sensations without emotional reactivity, which lessens both physical discomfort and mental distress. 10
Physical activity, especially gentle exercises like yoga or walking, releases endorphins that naturally reduce pain perception and improve mental clarity, acting as a powerful tool for both body and mind. 11
Support groups offer psychological comfort, validation, and coping tips from others facing similar struggles, helping to relieve the emotional burden of feeling alone in chronic pain journeys. 12
Patients often report a cycle where pain increases stress, and stress further increases pain, suggesting that managing mental health is critical to breaking this harmful feedback loop. 13
Journaling thoughts and tracking symptoms has helped many identify pain patterns and triggers, offering a sense of control and therapeutic release that supports mental well-being. 14

Biofeedback therapy trains people to control physiological responses—like heart rate and muscle tension—improving pain tolerance and fostering emotional regulation through measurable progress.
Nutrition and hydration affect chronic pain and mental health more than many realize, as deficiencies in certain vitamins (like B12 or magnesium) can worsen fatigue and emotional symptoms. 15
Acceptance and Commitment Therapy (ACT) helps patients embrace pain as part of life rather than resist it, leading to improved psychological flexibility and reduced emotional suffering. 16
Psychologist Viktor Frankl believed meaning helps overcome suffering. Similarly, chronic pain patients who pursue purpose—even small goals—often report greater resilience and emotional strength in their pain journey. 17


