“
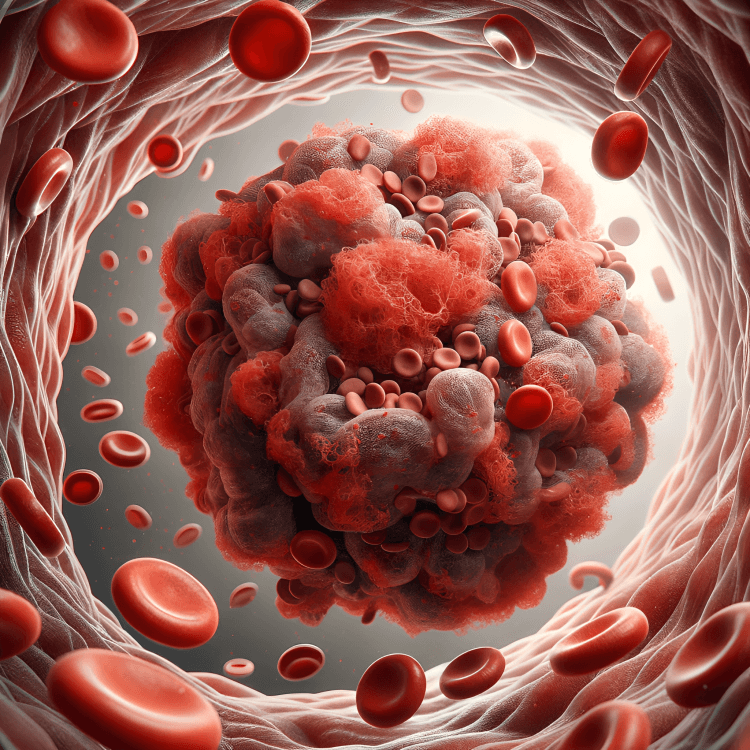
Risk Factors for Deep Vein Thrombosis (DVT) is a serious medical condition that occurs when a blood clot forms in a deep vein, usually in the legs. By learning about them, individuals can take proactive steps to reduce the likelihood of DVT and avoid life-threatening complications such as pulmonary embolism. 1
1
”
Prolonged sitting during air travel or car rides can cause blood flow to stagnate, especially in the legs, increasing the likelihood of clot formation in deep veins of the lower body. 1
A family history of clotting disorders or DVT significantly raises the chances of developing deep vein thrombosis, even in individuals with an otherwise healthy lifestyle or normal medical background. 2
Being overweight or obese puts extra pressure on leg veins, which slows blood flow and raises the risk of clot formation, especially when combined with inactivity or hormonal factors. 3
Smoking damages the inner lining of blood vessels and increases blood thickness, both of which contribute to conditions favorable for the development of deep vein thrombosis.
Women taking birth control pills or undergoing hormone replacement therapy have elevated levels of estrogen, which can lead to increased clotting potential and higher chances of DVT. 4
Pregnancy increases pressure in the pelvic veins and causes hormonal shifts that promote clotting, making pregnant women particularly susceptible to DVT, especially in the third trimester or postpartum period. 5
Individuals who undergo major surgery, especially hip or knee replacement, face a high risk of DVT due to blood vessel injury, inflammation, and extended recovery immobility. 6
Cancer and its treatments, including chemotherapy, can alter blood composition and damage vessels, dramatically raising the chances of blood clot development within deep veins. 7
People over the age of 60 face an increased risk of DVT due to reduced mobility, vein elasticity loss, and changes in blood chemistry that promote clot formation. 8

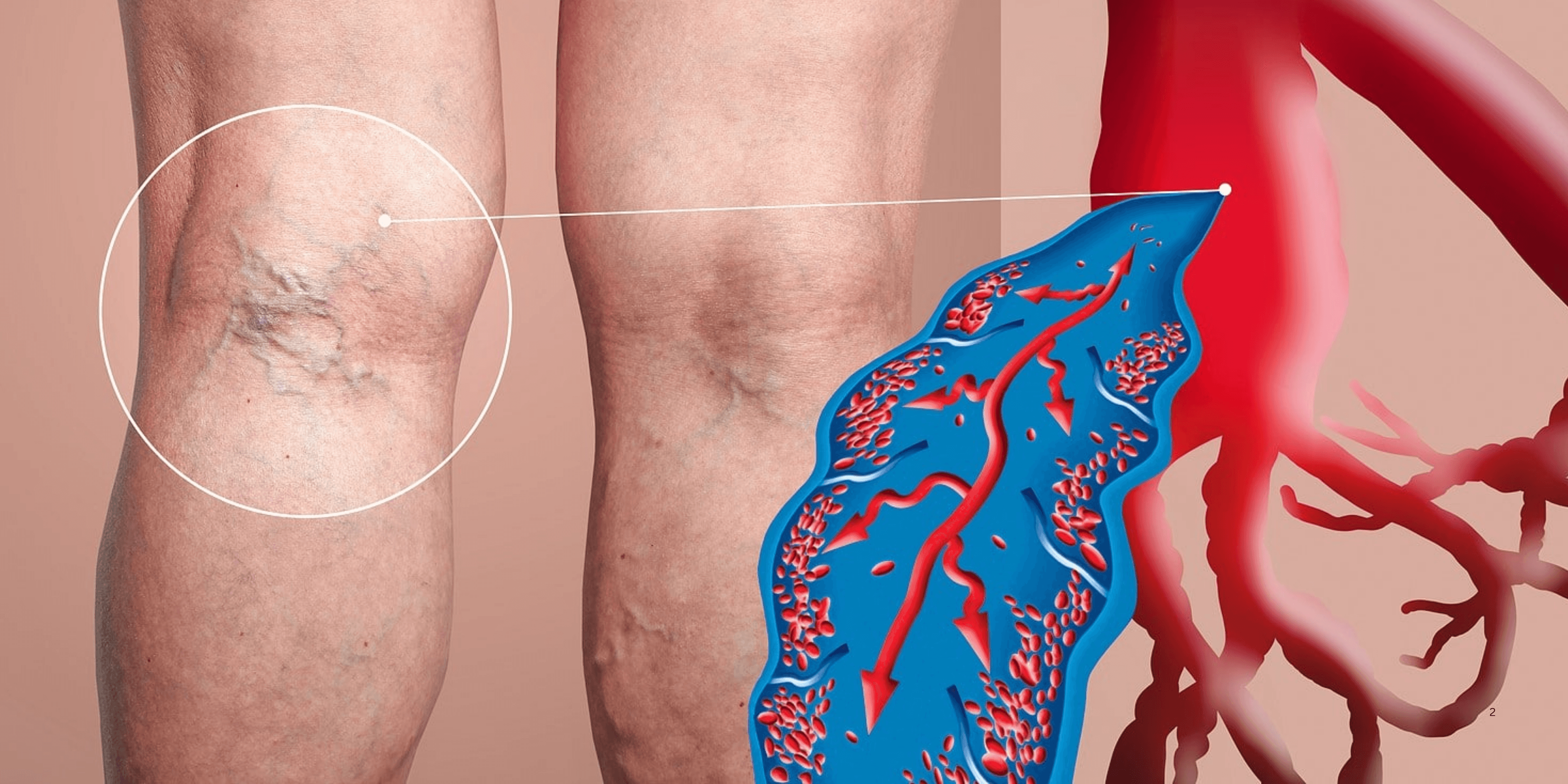
Varicose veins, though often seen as a cosmetic issue, are a recognized risk factor for DVT because they indicate poor circulation and weakened vein walls that can contribute to clot development.
Long-term use of central venous catheters or IV lines may irritate or damage vein walls, leading to clot formation around the catheter site or in deep veins over time. 9
Chronic heart failure can slow blood flow and reduce the efficiency of circulation, which increases the likelihood of clotting in the deep veins of the legs. 10
Autoimmune diseases like lupus and antiphospholipid syndrome can trigger abnormal clotting mechanisms, raising the risk of deep vein thrombosis in affected individuals. 11
Trauma to the lower limbs or pelvis—such as fractures, dislocations, or direct impacts—can injure blood vessels, creating the perfect conditions for deep clots to form during healing. 12
Dehydration reduces blood volume and increases its thickness, which slows circulation and can promote clot formation under certain physical or environmental stress conditions. 13
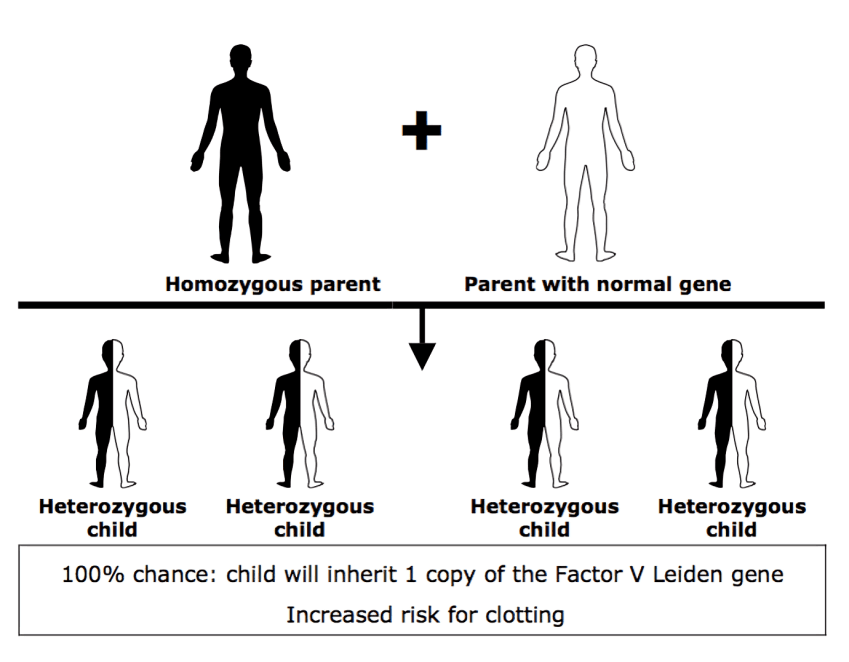
Some individuals have inherited clotting disorders, such as the Factor V Leiden mutation, which makes their blood more prone to clotting even without common environmental or lifestyle triggers.
Certain infections can cause systemic inflammation and damage to blood vessels, raising the risk of deep clots, particularly in hospitalized or immunocompromised individuals. 14
Flight attendants, truck drivers, and office workers with sedentary work routines are among occupational groups at increased risk due to limited leg movement over extended hours. 15
Tight clothing around the thighs or waist can impede circulation over time, especially when paired with prolonged sitting or underlying vascular issues, subtly contributing to clot risk. 16
Sir William Osler, a pioneer in modern medicine, emphasized the connection between immobility and blood stasis long before imaging technology confirmed these risks in diagnosing deep vein thrombosis. 17


