
“
Understanding the signs of bipolar disorder in adults is vital for timely diagnosis and care. These mood swings often go beyond ordinary emotional ups and downs. Recognizing the signs of bipolar disorder in adults can guide early treatment, helping individuals live balanced and fulfilling lives. 1
1
”
Adults with bipolar disorder often experience alternating periods of intense emotional highs (mania or hypomania) and profound lows (depression), which can harm relationships, work, mood, and daily tasks. 1
During manic episodes, people may feel euphoric, extremely energetic, or unusually irritable. This intense mood shift can lead to impulsive decisions, hyperactivity, and risky behaviors that are often harmful. 2
Depressive episodes bring persistent sadness, emptiness, or hopelessness. These feelings often cause a loss of interest in favorite activities and make it difficult to concentrate or even get out of bed in the morning. 3
A reduced need for sleep is common in mania, where someone might feel fully rested after only two or three hours. On the flip side, depression may cause severe insomnia or excessive sleeping throughout the day. 4
Rapid speech and racing thoughts are signs of a manic state. The person might speak in a pressured way, jumping between unrelated topics, making conversations chaotic and extremely hard to follow by others.
Impulsive behaviors like reckless spending, fast driving, or engaging in unsafe sex are typical in manic phases. These choices often result in financial issues, health risks, or broken relationships after the episode ends. 5
During depressive episodes, a person may experience feelings of worthlessness, extreme guilt, or self-loathing. These mental states can sometimes lead to suicidal ideation or harmful behaviors. 6
Psychotic symptoms like hallucinations or delusions can occur in severe manic or depressive states. These experiences often lead to misdiagnosis as schizophrenia or severe depression with psychotic features. 7
The duration of mood episodes can differ greatly among individuals. Some may experience several episodes per year, while others go months without symptoms. Rapid cycling involves four or more episodes within a single year. 8
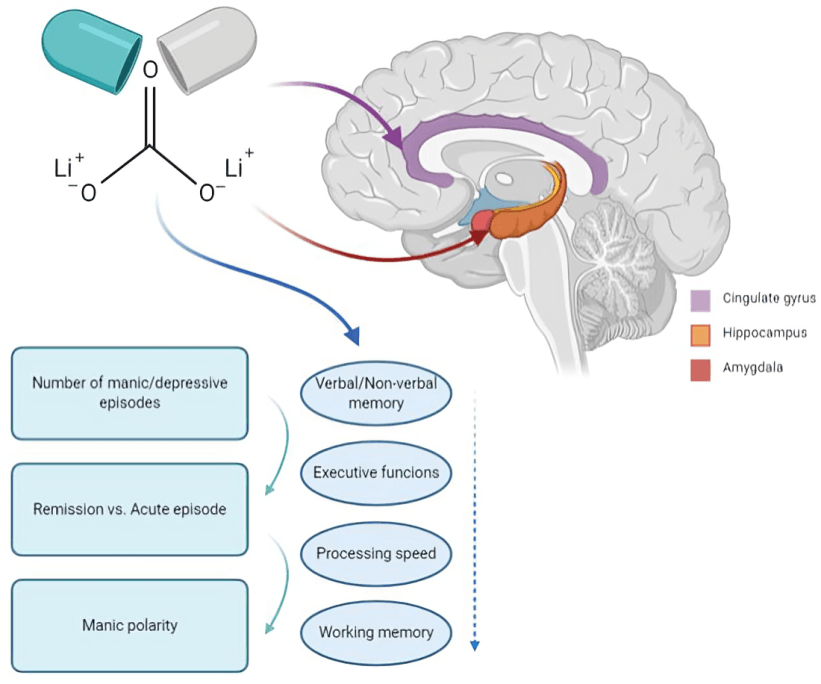
Bipolar disorder often affects cognition. Memory lapses, poor concentration, and indecisiveness are common during both mania and depression, making tasks like working or studying incredibly difficult to manage.
Irritability and agitation can dominate both mood states. Someone in a manic or depressive phase might seem short-tempered, aggressive, or overly reactive, leading to frequent arguments or social isolation. 9
Changes in appetite and weight often signal a mood episode. Manic individuals might eat more or indulge in junk food, while depressed people usually experience appetite loss and disinterest in eating. 10
Grandiosity—an inflated sense of self-worth—is a classic manic symptom. A person may believe they have special powers, superior talents, or are destined for fame, even in the absence of any real evidence. 11
Depressive phases can cause physical symptoms like body aches, slowed movements, or constant fatigue. These signs are sometimes misinterpreted as physical illness, delaying a correct psychiatric diagnosis. 12

People with bipolar disorder often struggle with substance abuse. Alcohol and drugs might be used to self-medicate mood swings but instead worsen symptoms and interfere with prescribed treatment plans.
Seasonal changes may influence mood cycles in bipolar individuals. Depression may worsen during winter months, while hypomanic or manic episodes often arise during spring or summer, sometimes without clear triggers. 13
Family history is a major risk factor. If a parent or sibling has bipolar disorder, the likelihood of developing it significantly increases, emphasizing the importance of genetic and hereditary understanding. 14
Traumatic life events such as abuse, the death of a loved one, or major career setbacks can trigger episodes. Managing stress through therapy or lifestyle changes helps prevent emotional instability. 15
Diagnosing bipolar disorder requires a thorough clinical evaluation. Mental health professionals often consider mood patterns, life history, family input, and sometimes medical tests to rule out other disorders. 16
Long-term care is crucial, involving regular appointments and monitoring. Mental health professionals track progress, adjust medications, and provide support, helping individuals maintain stability and avoid relapse over time.17


