
“
Substance abuse and depression are often deeply interconnected, creating a cycle that can be difficult to break. Many individuals struggling with substance abuse also face depression, and vice versa, making treatment and recovery complex but essential. Understanding the link between substance abuse and depression can provide insights into effective intervention strategies.1
1
”
Substance abuse and depression are linked, with individuals using drugs or alcohol to self-medicate. This worsens depression over time, creating a cycle that is difficult to break. 1
Depression and substance abuse can worsen each other. Substance use intensifies depression, while depression increases the need for substances, creating a dangerous cycle. 2
Individuals with both depression and substance abuse face more severe challenges. Co-occurring conditions are harder to treat and require specialized therapy for effective management.
Many people with depression misuse substances to cope with sadness and hopelessness. Alcohol or drugs provide temporary relief but deepen the depression over time. 3
Depression increases the risk of substance abuse. It creates feelings of worthlessness, prompting individuals to use substances as temporary relief, which only worsens their condition. 4
Depression can alter brain chemistry, making people more susceptible to addiction. Chronic substance use further disrupts brain function, complicating mental health management. 5
People with depression may abuse alcohol, marijuana, or prescription drugs. These substances provide temporary relief but can worsen depression and lead to addiction. 6
Depression can increase cravings for substances. Many people use alcohol or drugs to numb negative emotions, but the relief is temporary and often leads to increased dependency. 7
Depression lowers motivation and energy, making it harder to stop using substances. This leads to a cycle where depression encourages more substance abuse and vice versa. 8
Long-term substance abuse can worsen depression. Alcohol and narcotics interfere with neurotransmitter production, which regulates mood, leading to more intense depressive episodes. 9

Treating both depression and substance abuse requires a dual-diagnosis approach. Therapies like cognitive-behavioral therapy (CBT) and medication-assisted treatment (MAT) offer the best recovery chances.
Substance abuse and depression are common in individuals who’ve experienced trauma. Drugs and alcohol serve as coping mechanisms, often deepening the depression linked to past experiences. 10
Genetics contribute to both depression and addiction. People with a family history of either condition are more likely to struggle with both, creating a complicated mental health scenario. 11
Depression can be triggered or worsened by substance abuse. Alcohol and narcotics disrupt neurotransmitters, leading to hopelessness and anxiety, which deepen depression. 12
Both depression and substance abuse often lead to poor self-care. Neglecting nutrition, sleep, and exercise worsens both conditions, making recovery harder and leading to physical health problems. 13
Depression increases the severity of substance abuse. People rely more on substances to cope with low mood, leading to greater dependency and more intense depressive symptoms. 14
Stress exacerbates the link between depression and substance abuse. High stress triggers depressive episodes and cravings for substances, reinforcing the cycle of self-medication. 15
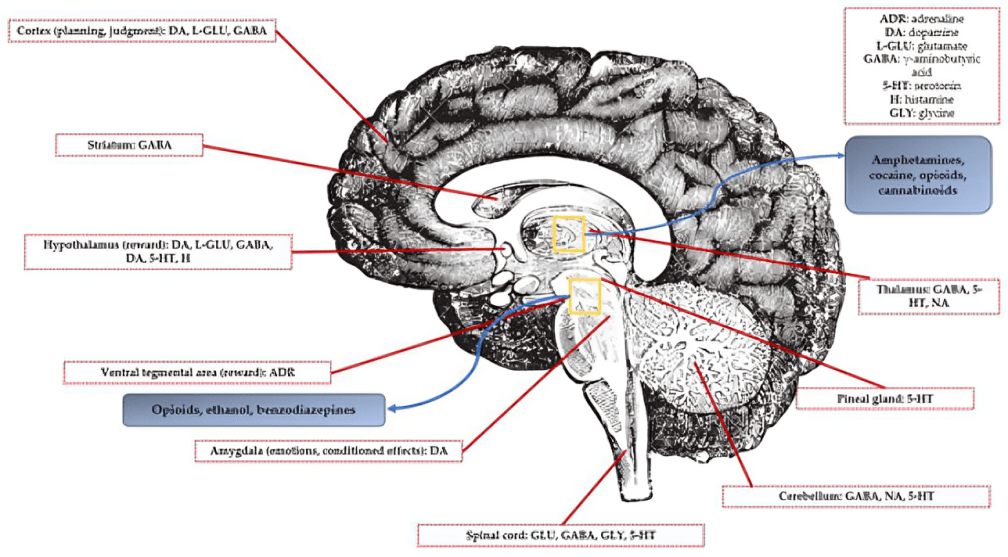
Illicit substances, especially stimulants like cocaine, cause mood swings that mimic or worsen depression. These substances alter brain chemistry, creating emotional instability.
Depression makes it harder for individuals to seek treatment for substance abuse. Low motivation can prevent them from accessing help, prolonging the struggle with both conditions. 16
Substance abuse programs often address both depression and addiction. Treating depression alongside substance abuse improves recovery chances by tackling the root causes of both conditions. 17


